Every year in France, 140,000 people suffer a stroke. © Adobe Stock
Each year in France, 140,000 people are victims of a stroke.[1]. About 80% of them are cerebral infarctions or ischemic strokes, linked to the occlusion of a cerebral artery by a blood clot. Studies have shown that the risk of ischemic stroke is increased by taking antipsychotics, drugs with antidopaminergic properties[2] commonly prescribed in psychiatry. Researchers from Inserm and the University of Bordeaux (Bordeaux Population Health Research Center), and Bordeaux University Hospital, assessed the risk of ischemic stroke associated with exposure to other antidopaminergic drugs: antiemetics, drugs very commonly used in the symptomatic treatment of nausea and vomiting. The results of this study, obtained through the analysis of national health insurance reimbursement data, highlight an association between taking these drugs and the risk of having an ischemic stroke. They are published in the British Medical Journal.
Since the early 2000s, taking antipsychotic drugs indicated in psychiatry has been associated with an increased risk of ischemic stroke. This risk has been demonstrated for all of these medicinal products with antidopaminergic properties; it increases with age and the presence of dementia. The underlying mechanisms are not elucidated, the antidopaminergic action is a possible hypothesis. Antiemetics -domperidone, metoclopramide and metopimazine- used in the symptomatic treatment of nausea and vomiting of various origins (acute gastroenteritis, migraine, post-operative context or in the context of chemo- or radiotherapy) are other drugs with this property.
To date, no study has been published evaluating the risk of ischemic stroke associated with exposure to antidopaminergic antiemetics. These drugs are however used very commonly: in 2017 in France, more than 4 million people had at least one reimbursement for metopimazine, the most used of them.
Researchers from Inserm, the University of Bordeaux and the Bordeaux University Hospital have taken an interest in this risk. They did a study[3] so-called “own-control case” using the reimbursement data of the Health Insurance and those of hospital admissions. In this type of study, the potential use of the drug in the period immediately preceding the accident (here 14 days) is compared with the same use during an earlier period (here more than a month) where it cannot have caused the event. A stronger use in the period immediately preceding the accident is in favor of a role played by the drug in the attack.
This method makes it possible to automatically take into account personal risk factors for ischemic stroke, such as smoking, body mass index, physical activity, or eating habits. Other factors likely to vary over the short follow-up time in the same individual have been considered, including the use of drugs that are risk factors for stroke (such as vasoconstrictors) or, on the contrary, that protect against this risk (anticoagulants, antiaggregants platelets).
The study thus initially analyzed the data for 2,612 adults hospitalized for a first ischemic stroke and having started treatment with antiemetics in the 70 days preceding the ischemic stroke. In these subjects, the analyzes found a higher consumption of antiemetics in the days preceding the stroke marked by a peak in treatment initiation over this period. This result suggests that there would be an increased risk of ischemic stroke at the start of use of these drugs (Figure below).
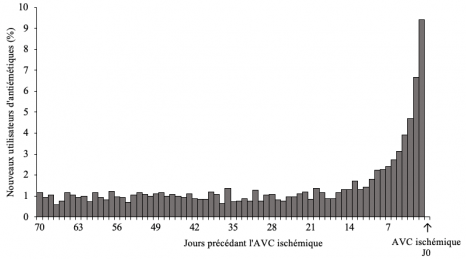
Distribution of initiation of antiemetics during the 70 days preceding the onset of ischemic stroke (N=2,612 subjects with ischemic stroke).
To eliminate a bias in the results that could arise if the use of the drug varied greatly over time in the general population (for example, during epidemics of acute gastroenteritis), the study then considered , over the same period, a random group of 21,859 people who had not had a stroke. In these people, no peak or excess of use of antiemetics comparable to that highlighted in patients who presented a CVA was found (Figure below).
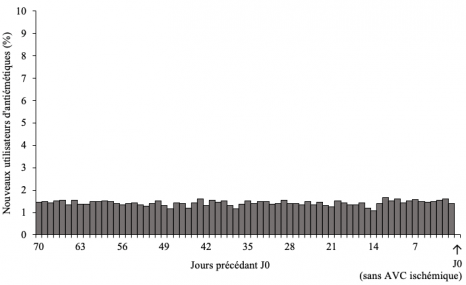
Distribution of the initiation of antiemetics during the 70 days preceding the reference date (N= 21,859 subjects who did not present with an ischemic stroke).
The results of this study suggest an increased risk of ischemic stroke in the first days of use of antidopaminergic antiemetic drugs. This increased risk was found for the three antiemetics studied -domperidone, metoclopramide and metopimazine-, and the risk appeared to be higher in the first days of use.
“This first study provides a strong signal, relating to drugs widely used in the general population. For the time being, it seems very important that these results can be replicated in other studies, studies which could also provide indications on the frequency of this adverse effect, which we could not measure here given the approach methodology adopted. Having precise information on the subtypes of ischemic strokes and their location would also make it possible to explore the mechanisms involved,” explains Anne Bénard-Laribière, one of the authors of the study.
[1] Cerebrovascular accident (CVA), the leading cause of acquired disability in adultsInserm, 2019
[2] Antidopaminergics block the action of dopamine, a neurotransmitter involved, among other things, in regulating behavior, but also muscle tone and movement coordination.
[3] This study was carried out within the framework of the work program of the DRUGS-SAFE CenterRfunded by the ANSM and partner of the GIS EPI-PHARE.