The Silent Epidemic Evolving: How MASLD is Set to Reshape Liver Health and Beyond
Imagine a condition affecting nearly a third of the global population, yet remaining largely unknown even to those diagnosed. That’s the reality of Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD), formerly known as Non-Alcoholic Fatty Liver Disease (NAFLD). A recent surge in diagnoses, like that of Hong Kong teacher Nalini Lakhani, is highlighting a critical shift in understanding – and a looming public health challenge. But this isn’t just about a name change; it’s about recognizing liver disease as a systemic metabolic issue, and preparing for a future where personalized prevention and treatment are paramount.
From NAFLD to MASLD: Why the Shift Matters
For years, NAFLD was considered a disease of exclusion – a diagnosis given when other causes of liver fat accumulation were ruled out. However, research increasingly pointed to metabolic dysfunction – conditions like obesity, type 2 diabetes, and dyslipidemia – as the primary drivers. The 2020 shift to MASLD reflects this understanding, emphasizing that the liver isn’t the *problem*, but rather a *victim* of broader metabolic imbalances. Dr. Loey Mak Lung-yi, a Hong Kong-based specialist, notes the diagnostic overlap is significant – a 95% similarity – but the focus on metabolic factors opens doors to more targeted interventions.
Understanding the Metabolic Roots
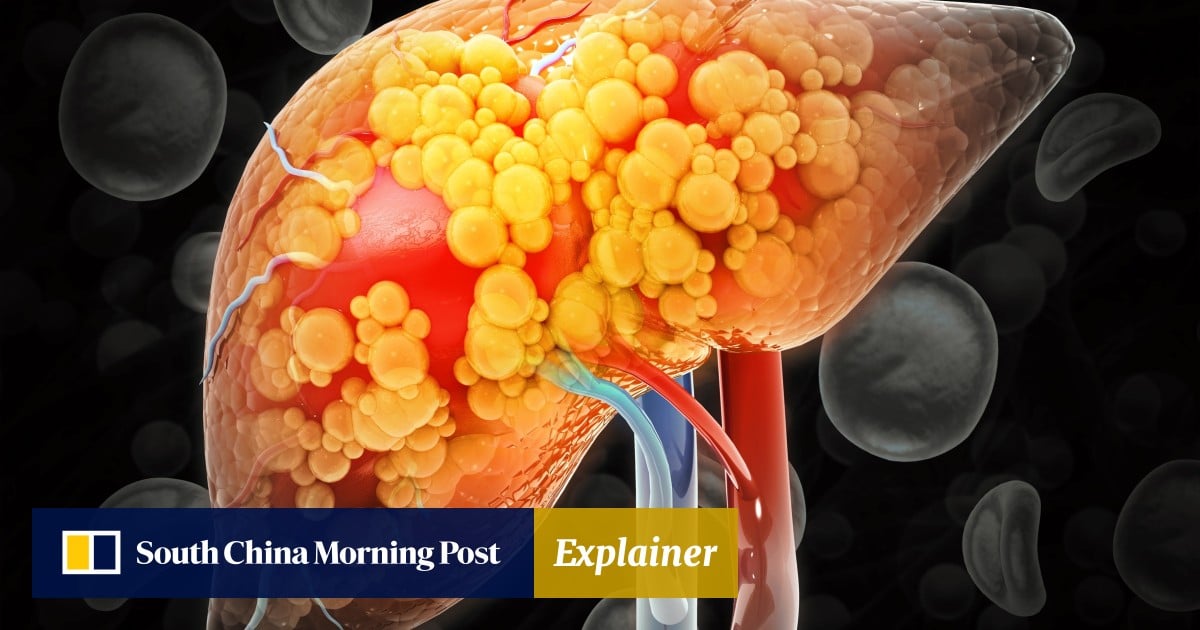
MASLD isn’t simply about excess fat in the liver (defined as more than 5% of the liver’s weight). It’s intricately linked to insulin resistance, inflammation, and altered lipid metabolism. Dyslipidemia, characterized by abnormal levels of fats in the blood, plays a crucial role. High triglycerides and low HDL cholesterol are common indicators, signaling a disruption in how the body processes and utilizes fats. This metabolic cascade can lead to steatosis (fat accumulation), steatohepatitis (inflammation), fibrosis (scarring), and ultimately, cirrhosis and liver cancer.
The Future Landscape of MASLD: Trends to Watch
The evolution of MASLD isn’t just a medical reclassification; it’s a catalyst for several key trends that will reshape liver health in the coming years.
1. Rise of Non-Invasive Diagnostics
Currently, liver biopsy is the gold standard for diagnosing and staging MASLD. However, it’s invasive, costly, and carries risks. The future lies in non-invasive diagnostic tools. Researchers are actively developing and refining techniques like:
- FibroScan: Uses ultrasound to measure liver stiffness, indicating the degree of fibrosis.
- Blood Biomarkers: Identifying specific proteins and metabolites that correlate with MASLD severity.
- AI-Powered Imaging: Utilizing artificial intelligence to analyze medical images (MRI, CT scans) for subtle signs of liver disease.
These advancements will enable earlier detection, wider screening, and more personalized management of MASLD.
2. Personalized Medicine Takes Center Stage
Recognizing MASLD as a metabolic disease necessitates a personalized approach. A “one-size-fits-all” strategy won’t work. Future treatment plans will increasingly consider:
- Genetic Predisposition: Identifying individuals at higher risk based on their genetic makeup.
- Gut Microbiome Analysis: Understanding the role of gut bacteria in metabolic dysfunction and tailoring interventions accordingly.
- Lifestyle Factors: Developing individualized diet and exercise plans based on a patient’s specific needs and preferences.
Expert Insight: “We’re moving away from simply treating the liver and towards addressing the underlying metabolic drivers of the disease,” says Dr. Anya Sharma, a leading researcher in metabolic liver disease. “This requires a holistic approach that considers the patient as a whole.”
3. The Pharmaceutical Pipeline Heats Up
While lifestyle modifications remain the cornerstone of MASLD management, the pharmaceutical industry is actively developing new drugs targeting various aspects of the disease. Several promising therapies are in clinical trials, including:
- PPAR Agonists: Drugs that improve insulin sensitivity and reduce liver fat.
- GLP-1 Receptor Agonists: Originally developed for diabetes, these drugs have shown potential in reducing liver inflammation and fibrosis.
- ACC Inhibitors: Targeting a key enzyme involved in fat synthesis.
Expect to see a growing number of pharmaceutical options available in the coming years, offering hope for patients who don’t respond adequately to lifestyle changes.
4. MASLD and the Cardiovascular Connection
MASLD isn’t just a liver disease; it’s a systemic condition with strong links to cardiovascular disease. Patients with MASLD are at increased risk of heart attack, stroke, and other cardiovascular events. This connection is driving a greater emphasis on integrated care, with collaboration between hepatologists and cardiologists becoming increasingly common. Future strategies will focus on addressing both liver and cardiovascular risk factors simultaneously.
Actionable Steps You Can Take Now
Even as research and treatment options evolve, there are proactive steps you can take to protect your liver health:
Pro Tip: Limit your intake of processed foods, sugary drinks, and saturated fats, as these can contribute to metabolic dysfunction.
Did you know? Even modest weight loss (5-10% of body weight) can significantly improve liver health in individuals with MASLD.
Frequently Asked Questions
Q: Is MASLD reversible?
A: In many cases, yes. Early intervention with lifestyle modifications can often reverse steatosis and even reduce inflammation. However, advanced fibrosis and cirrhosis may not be fully reversible.
Q: Who is at risk for MASLD?
A: Individuals with obesity, type 2 diabetes, dyslipidemia, metabolic syndrome, and a family history of liver disease are at increased risk.
Q: What are the symptoms of MASLD?
A: MASLD is often asymptomatic in its early stages. Symptoms may include fatigue, abdominal discomfort, and elevated liver enzymes detected during routine blood tests.
Q: How often should I get screened for MASLD?
A: If you have risk factors for MASLD, discuss screening options with your doctor. Regular checkups and blood tests can help detect the condition early.
The story of Nalini Lakhani serves as a powerful reminder: awareness is the first step. As our understanding of MASLD deepens, and new diagnostic and therapeutic tools emerge, we’re poised to tackle this silent epidemic and safeguard liver health for generations to come. What lifestyle changes will *you* commit to today to support your metabolic health?